The ACA, which is often referred to as Obamacare, experienced high enrollments during the registration period for 2017. This year, there is an abbreviated period for signing up to be insured beginning on Jan. 1, 2018.
Last year the dates for open enrollment were November 1-January 31. However, this year the closing date is December 15, which is also the time frame used for Medicare and Medicare Part D applicants each year.
There are special circumstances that will allow people to sign up at different times. The special enrollment period (SEP) for those most affected by Hurricanes Irma and Harvey the deadline is December 31. The people allowed this special time frame include:
- All of those living in Florida.
- The residents of Camden, Charlton, Chatham, Coffee, Glynn, Liberty, McIntosh counties in Georgia.
- Those living in 47 of the 254 counties in Texas qualify for the extension. These are located in the Gulf Coast region from Sabine to the north and Kleberg in the south. For a full list go to the FEMA website.
Others might qualify for the SEP with the required proof of need. While not regulated by the ACA, if a person needs to know if they are allowed to apply outside of the standard period should go to the Health Insurance website (healthinsurance(dot)org). However, there are standard events that will allow for a SEP under specified rules:
- An income increase that moves a person out of the coverage gap,
- Employer-sponsored coverage reducing benefits such that it no longer provides minimum value, or becomes unaffordable,
- A permanent move to an area where different qualified health plans (QHPs) are available,
- Becoming a citizen of the United States,
- Marriage,
- Divorce,
- Becoming a dependent or gaining a dependent as a result of birth, adoption, or placement in foster care,
- Involuntary loss of other coverage,
- Individual plan renewing outside of the regular open enrollment,
- An error or problem with enrollment.
A person could lose their coverage if they have a wage increase that removes their eligibility for the coverage gap. People who fall into this category are those with incomes that fall below the poverty line and do not qualify for Medicaid.
While this seems improbable it is not, a family of three bringing home less than the poverty level, but more than allowed for Medicaid. Another reason would be residing in a state does not allow single dependentless low-income adults become Medicaid recipients.
To remain insured in 2018 there is nothing to do. However, if a person wants to change the plan they for which are currently enrolled or a new ACA applicant they must do so between November 1-December 15.
Everyone should be notified of this change since enrollment period was cut in half. It is important to remember and share this information because late registrations will not be accepted. Moreover, proof must be provided to qualify for a Special Enrollment Period application.
By Cathy Milne
Sources:
Health Insurance: What’s the deadline to get coverage during Obamacare’s open enrollment period?
Health Insurance: Qualifying events that can get you coverage
Families USA: A 50-State Look at Medicaid Expansion
Featured Image Courtesy of Kristina Hernandez’s Flickr Page – Creative Commons License
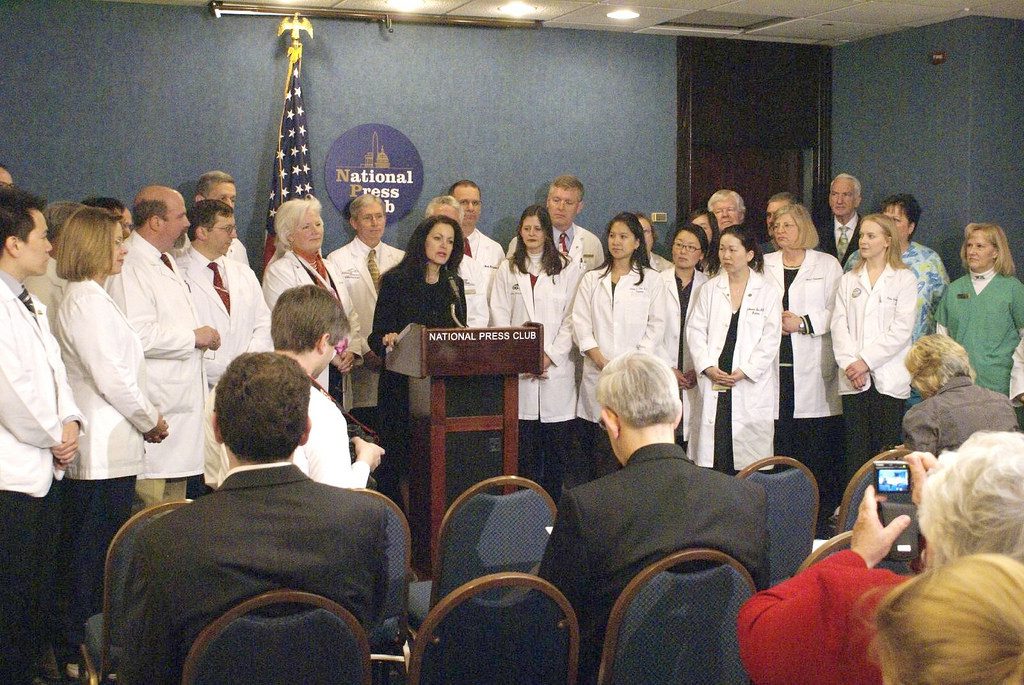
Top Image Courtesy of Ted Eytan’s Flickr Page – Creative Commons License